Listen to this article
Produced by ElevenLabs and News Over Audio (NOA) using AI narration.
When scientists first created the class of drugs that includes Ozempic, they told a tidy story about how the medications would work: The gut releases a hormone called GLP-1 that signals you’re full, so a drug that mimics GLP-1 could do the exact same thing, helping people eat less and lose weight.
The rest, as they say, is history. The GLP-1 revolution birthed semaglutide, which became Ozempic and Wegovy, and tirzepatide, which became Mounjaro and Zepbound—blockbuster drugs that are rapidly changing the face of obesity medicine. The drugs work as intended: as powerful modulators of appetite. But at the same time that they have become massive successes, the original science that underpinned their development has fallen apart. The fact that they worked was “serendipity,” Randy Seeley, an obesity researcher at the University of Michigan, told me. (Seeley has also consulted for and received research funding from companies that make GLP-1 drugs.)
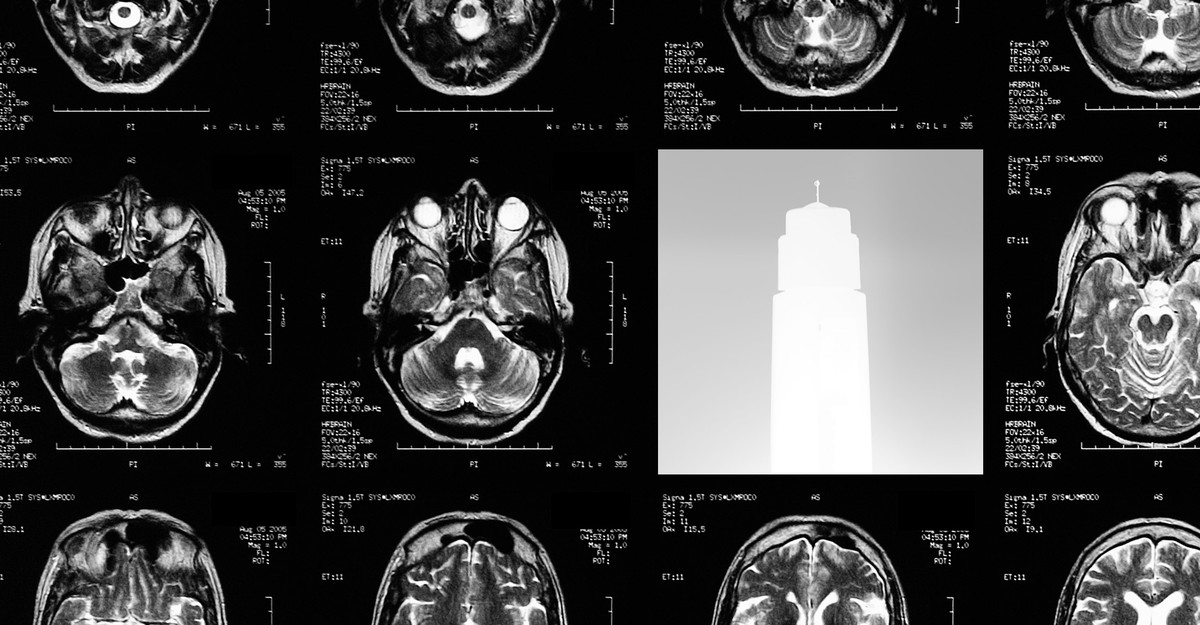
Now scientists are beginning to understand why. In recent years, studies have shown that GLP-1 from the gut breaks down quickly and has little effect on our appetites. But the hormone and its receptors are naturally present in many parts of the brain too. These brain receptors are likely the reason the GLP-1 drugs can curb the desire to eat—but also, anecdotally, curb other desires as well. The weight-loss drugs are ultimately drugs for the brain.
Obesity medications differ in a key way from the natural molecule they’re meant to mimic: They last a lot longer. GLP-1 released in the gut has a half-life of just minutes in the bloodstream, whereas semaglutide and tirzepatide have half-lives measured in days. This is by design. Both drugs were specifically engineered to resist degradation, so that they need to be injected only once a week. (The very first GLP-1 drug on the market, exenatide, had to be injected twice a day when it was released, in 2005—the field has come a long way.) The medications are also given at levels much higher than natural GLP-1 ever reaches in the bloodstream; Seeley tends to put it at five times as high, but he said even that may be a gross underestimate.
By indiscriminately flooding the body with long-lasting molecules, the injections likely allow engineered GLP-1 drugs to penetrate parts of the body that the natural gut hormone cannot—namely, deep in the brain. First-generation GLP-1 drugs including exenatide, which are far less powerful than the current crop, have been shown to cross the blood-brain barrier and tickle areas important for appetite and nausea. Exactly what Ozempic and its successors do is still less clear, but they are so effective that many scientists think they must be reaching far, directly or indirectly.
All of this matters because the brain, as we now know, has its own GLP-1 system, parallel to and largely separate from whatever is going on in the gut. Neurons in the hindbrain, sitting at the base of the skull, secrete their own GLP-1, while receptors listening to them are found throughout the brain. In animal experiments, hitting those receptors indeed suppresses appetite.
It took a long time for scientists to appreciate the extent of GLP-1 in the brain, Karolina Skibicka, a neuroscientist at Penn State, told me. When she published her first study, in 2012, on a GLP-1 drug’s impact on the dopamine reward system, she had to spend two years going back and forth with skeptical reviewers. At the time, she said, “the idea was considered so wild.” (Skibicka has received research funding from the Novo Nordisk Foundation, which has a majority ownership in but whose grants are commercially independent from Novo Nordisk, the manufacturer of Ozempic.) Since then, in a series of clever experiments using rodents, scientists have been able to show that GLP-1 drugs likely act on the brain. They don’t seem to work, for example, to suppress appetite in mice whose brain GLP-1 receptors have been genetically erased. Moreover, the effects of GLP-1 extend beyond food: Rodents given the drugs will drink less alcohol and use less cocaine. Anecdotally, too, people on GLP-1 medications have reported spontaneously quitting drinking, smoking, shopping, and other addictive and compulsive behaviors.
A more refined understanding of how GLP-1 works in the brain could help improve the current injections. Nausea and vomiting are among the most common side effects and would seem to go hand in hand with a lack of appetite. But these symptoms appear to be governed by distinct systems in the brain, Scott Kanoski, a neuroscientist at the University of Southern California, told me. In fact, scientists have been able to find brain areas in rodents where GLP-1 analogs can suppress appetite without causing nausea, which hints at the possibility of developing drugs that do the same.
Even as scientists zero in on the likely mechanisms of these weight-loss drugs, they are encountering new and baffling questions. Tirzepatide, for example, activates receptors for a second hormone called GIP, and this is often cited as a potential explanation for its slightly superior efficacy over semaglutide, which acts on GLP-1 alone. But just last month, Amgen released data on a new drug that activates GLP-1 receptors, blocks GIP receptors, and still helps people lose weight. How can two drugs with opposite actions on GIP have the same outcome?
Scientists are perplexed, but they are not shocked. For years and years, promising findings in rats and mice did not translate into real-world treatments for obesity. Drugs based on other, seemingly important hormones—ghrelin (the “hunger hormone”) and leptin (the “satiety hormone”)—were never able to achieve the spectacular clinical results of GLP-1. The latest drugs succeeded not because we fully understood the hormone they’re based on but because we got lucky. And drug development, for all the careful research required, does sometimes come down to luck.
In the end, gut GLP-1 could still be important—just not for appetite regulation. The stuff that is produced by the gut, specifically in the end of the small intestine and the colon, makes up most of the GLP-1 produced in the body, Daniel Drucker, an endocrinologist at Mount Sinai Hospital in Toronto, told me. It also tends to spike during gut infections. Drucker now thinks that GLP-1 in the gut is primarily responsible for controlling inflammation. (He has consulted for and received research funding from companies making GLP-1 drugs.) Other scientists have explored using GLP-1 drugs to treat inflammatory gut disease, such as ulcerative colitis and Crohn’s. But they’ve run into a bit of a dilemma: Many people with these conditions are already underweight, and GLP-1 drugs are just too good at making people lose more weight.