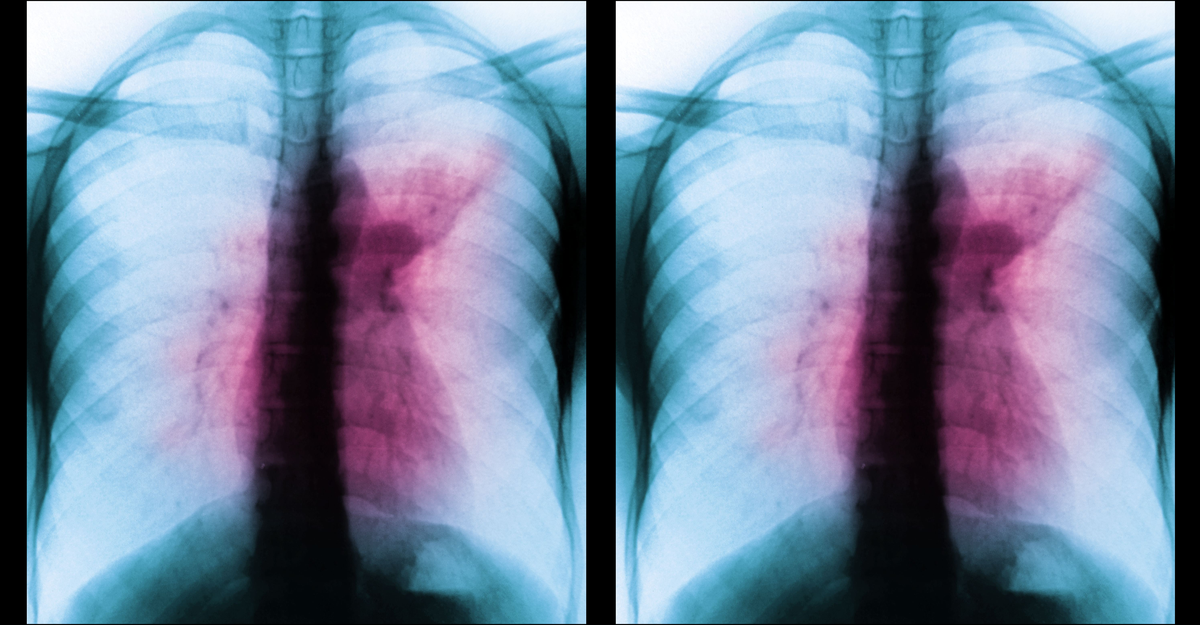
Growing up in India, which for decades has clocked millions of tuberculosis cases each year, Lalita Ramakrishnan was intimately familiar with how devastating the disease can be. The world’s greatest infectious killer, rivaled only by SARS-CoV-2, Mycobacterium tuberculosis spreads through the air and infiltrates the airways, in many cases destroying the lungs. It can trigger inflammation in other tissues too, wearing away bones and joints; Ramakrishnan watched her own mother’s body erode in this way. The sole available vaccine was lackluster; the microbe had rapidly evolved resistance to the drugs used to fight it. And the disease had a particularly insidious trait: After entering the body, the bacterium could stow away for years or decades, before erupting without warning into full-blown disease.
This state, referred to as latency, supposedly afflicted roughly 2 billion people—a quarter of the world’s population. Ramakrishnan, now a TB researcher at the University of Cambridge, heard that fact over and over, and passed it down to her own students; it was what every expert did with the dogma at the time. That pool of 2 billion people was understood to account for a large majority of infections worldwide, and it represented one of the most intimidating obstacles to eradicating the disease. To end TB for good, the thinking went, the world would need to catch and cure every latent case.
In the years since, Ramakrishnan’s stance on latent TB has shifted quite a bit. Its extent, she argues, has been exaggerated for a good three decades, by at least an order of magnitude—to the point where it has scrambled priorities, led scientists on wild-goose chases, and unnecessarily saddled people with months of burdensome treatment. In her view, the term latency is so useless, so riddled with misinformation, that it should disappear. “I taught that nonsense forever,” she told me; now she’s spreading the word that TB’s largest, flashiest number may instead be its greatest, most persistent myth.
Ramakrishnan isn’t the only one who thinks so. Together with her colleagues Marcel Behr, of Quebec’s McGill University, and Paul Edelstein, of the University of Pennsylvania (“we call ourselves the three BERs,” Ramakrishnan told me), she’s been on a years-long crusade to set the record straight. Their push has attracted its fair share of followers—and objectors. “I don’t think they’re wrong,” Carl Nathan, a TB researcher at Cornell, told me. “But I’m not confident they’re right.”
Several researchers told me they’re largely fine with the basic premise of the BERs’ argument: Fewer than 2 billion isn’t that hard to get behind. But how many fewer matters. If current latency estimates overshoot by just a smidge, maybe no practical changes are necessary. The greater the overestimate, though, the more treatment recommendations might need to change; the more research and funding priorities might need to shift; the more plans to control, eliminate, and eventually eradicate disease might need to be wholly and permanently rethought.
The muddled numbers on latency seem to be based largely on flawed assumptions about certain TB tests. One of the primary ways to screen people for the disease involves pricking harmless derivatives of the bacterium into skin, then waiting for an inflamed lump to appear—a sign that the immune system is familiar with the microbe (or a TB vaccine), but not direct proof that the bacterium itself is present. That means that positive results can guarantee only that the immune system encountered something resembling MTB at some point—perhaps even in the distant past, Rein Houben, an epidemiologist at the London School of Hygiene & Tropical Medicine, told me.
But for a long time, a prevailing assumption among researchers was that all TB infections had the potential to be lifelong, Behr told me. The thought wasn’t entirely far-fetched: Other microbial infections can last a lifetime, and there are historical accounts of lasting MTB infections, including a case in which a man developed tuberculosis more than 30 years after his father passed the bacterium to him. Following that logic—that anyone once infected had a good enough chance of being infected now—researchers added everyone still reacting to the bug to the pool of people actively battling it. By the end of the 1990s, Behr and Houben told me, prominent epidemiologists had used this premise to produce the big 2 billion number, estimating that roughly a third of the population had MTB lurking within.
That eye-catching figure, once rooted, rapidly spread. It was repeated in textbooks, academic papers and lectures, news articles, press releases, government websites, even official treatment guidelines. The World Health Organization parroted it too, repeatedly calling for research into vaccines and treatments that could shrink the world’s massive latent-TB cohort. “We were all taught this dogma when we were young researchers,” Soumya Swaminathan, the WHO’s former chief scientist, told me. “Each generation passed it on to the next.”
But, as the BERs argue, for TB to be a lifelong sentence makes very little sense. Decades of epidemiological data show that the overwhelming majority of disease arises within the first two years after infection, most commonly within months. Beyond that, progression to symptomatic, contagious illness becomes vanishingly rare.
The trio is convinced that a huge majority of people are clearing the bug from their body rather than letting it lie indefinitely in wait—a notion that recent modeling studies support. If the bacteria were lingering, researchers would expect to see a big spike in disease late in life among people with positive skin tests, as their immune system naturally weakens. They would also expect to see a high rate of progression to full-blown TB among people who start taking immunosuppressive drugs or catch HIV. And yet, neither of those trends pans out: At most, some 5 to 10 percent of people who have tested positive by skin test and later sustain a blow to their immune system develop TB disease within about three to five years—a hint that, for almost everyone else, there may not be any MTB left. “If there were a slam-dunk experiment, that’s it,” William Bishai, a TB researcher at Johns Hopkins, told me.
Nathan, of Cornell, was less sold. Immunosuppressive drugs and HIV flip very specific switches in the immune system; if MTB is being held in check by multiple branches, losing some immune defenses may not be enough to set the bacteria loose. But most of the experts I spoke with are convinced that lasting cases are quite uncommon. “Some people will get into trouble in old age,” Bouke de Jong, a TB researcher at the Institute of Tropical Medicine, in Antwerp, told me. “But is that how MTB hangs out in everybody? I don’t think so.”
If anything, people with positive skin tests might be less likely to eventually develop disease, Ramakrishnan told me, whether because they harbor defenses against MTB or because they are genetically predisposed to clear the microbe from their airway. In either case, that could radically change the upshot of a positive test, especially in countries such as the U.S. and Canada, where MTB transmission rarely occurs and most TB cases can be traced from abroad. Traditionally, people in these places with positive skin tests and no overt symptoms have been told, “‘This means you’ve got sleeping bacteria in you,’” Behr said. “‘Any day now, it may pop out and cause harm.’” Instead, he told me, health-care workers should be communicating widely that there could be up to a 95 percent chance that these patients have already cleared the infection, especially if they’re far out from their last exposure and might not need a drug regimen. TB drugs, although safe, are not completely benign: Standard regimens last for months, interact with other meds, and can have serious side effects.
At the same time, researchers disagree on just how much risk remains once people are a couple of years past an MTB exposure. “We’ve known for decades that we are overtreating people,” says Madhu Pai, a TB researcher at McGill who works with Behr but was not directly involved in his research. But treating a lot of people with positive skin tests has been the only way to ensure that the people who are carrying viable bacteria get the drugs they need, Robert Horsburgh, an epidemiologist at Boston University, told me. That strategy squares, too, with the goal of elimination in places where spread is rare. To purge as much of the bug as possible, “clinicians will err on the side of caution,” says JoAnne Flynn, a TB researcher at the University of Pittsburgh.
Elsewhere in the world, where MTB transmission is rampant and repeat infections are common, “to be honest, nobody cares if there’s latent TB,” Flynn told me. Many people with very symptomatic, very contagious cases still aren’t getting diagnosed or treated; in too many places, the availability of drugs and vaccines is spotty at best. Elimination remains a long-term goal, but active outbreaks demand attention first. Arguably, quibbling about latency now is like trying to snuff stray sparks next to an untended conflagration.
One of the BERs’ main goals could help address TB’s larger issues. Despite decades of research, the best detection tools for the disease remain “fundamentally flawed,” says Keertan Dheda, a TB researcher at the London School of Hygiene & Tropical Medicine and the University of Cape Town. A test that could directly detect viable microbes in tissues, rather than an immune proxy, could definitively diagnose ongoing infections and prioritize people across the disease spectrum for treatment. Such a diagnostic would also be the only way to finally end the fuss over latent TB’s prevalence. Without it, researchers are still sifting through only indirect evidence to get at the global TB burden—which is probably still “in the hundreds of millions” of cases, Houben told me, though the numbers will remain squishy until the data improve.
That 2 billion number is still around—though not everywhere, thanks in part to the BERs’ efforts. The WHO’s most recent annual TB reports now note that a quarter of the world’s population has been infected with MTB, rather than is infected with MTB; the organization has also officially discarded the term latent from its guidance on the disease, Dennis Falzon, of the WHO Global TB Programme, told me in an email. However subtle, these shifts signal that even the world’s biggest authorities on TB are dispensing with what was once conventional wisdom.
Losing that big number does technically shrink TB’s reach—which might seem to minimize the disease’s impact. Behr argues the opposite. With a huge denominator, TB’s mortality rate ends up minuscule—suggesting that most infections are benign. Deflating the 2 billion statistic, then, reinforces that “this is one of the world’s nastiest pathogens, not some symbiont that we live with in peace,” Behr told me. Fewer people may be at risk than was once thought. But for those who are harboring the microbe, the dangers are that much more real.